The Customer at the Center of Healthcare's Attention
What do you consider the three main challenges of today’s Healthcare industry?
We need to look at the challenges of today’s healthcare industry from the lens of healthcare efficiency (Enhancing healthcare efficiency to achieve the Quadruple Aim):
a. Enhance Customer Experience (notice how we need to refer to stakeholders as a customer rather than as a member or a patient)
This is all about how healthcare needs to revolve around the customer rather than the member or patient moving about the different parts of the health ecosystem. Thus, instead of talking about the different healthcare service components such as a primary care doctor, specialist, hospital, lab, pharma/prescription drug etc., how do we make life simpler and easier and treat members and patients as customers, so they have better quality and satisfaction overall? Why do we still have to fill out paper forms each time we visit a dentist or a specialist or a hospital to describe all our allergies etc.? Shouldn’t the new interoperability measures make this easier and transparent, so data is automatically shared similar to how airlines transfer baggage from one airline to another? Why can’t we be informed of delays in appointments in advance instead of being made to wait in a hospital or a provider’s office?
b. Reduce per capita health care costs with better outcomes
According to the Centers for Medicare and Medicaid Services, the U.S. spent close to 20% of our Gross Domestic Product (GDP) on healthcare — and it’s projected to keep rising. However, society's needs are not just healthcare, there are other resource needs as well that will need to be looked at such as homelessness, food deserts etc. The goal should be to not only improve the health of the individual, so they don’t need repeated visits to the doctor but also when they do, they are affordable without compromising quality.
c. Improve care team well-being and productivity
According to Medscape’s annual Physician Lifestyle Report, 42% of physician respondents reported burnout due to overloaded work which can result in lower customer satisfaction, worse health outcomes, and possibly higher costs!
As the Institute of Health Care Improvement has stated, “For the health of our communities, for the health of our school systems, and the health of all our members”, we need to address all the 3 aspects above and also include the well-being of the care providers as well.
How will this paradigm shift towards Value-based Care affect the current execution of healthcare activities (from the providers to the payers)?
The shift towards value-based care should work to align incentives better. Currently, there is a lot of fragmentation, as Dr. Shrank said in an episode of Creating a New Healthcare:
Misaligned Incentives between payor, provider, and patients
Communication and coordination gaps between payors, providers, and patients.
Coordination gaps between healthcare delivery and social/behavioral health services
The slow spread of evidence-based healthcare innovations through and across healthcare delivery networks
Aligned incentives will lead to aligning the execution of healthcare activities optimally across payers and providers. Aligned incentives should lead to providers doing what they do best and healthcare payers doing what they do best with clearer boundaries and coordination.
Why should CxOs within health companies prioritize Chronic Diseases management and how would you advise them to take action on this?
In the US and countries with similar levels of development, Chronic Disease represents the largest cost avoidance opportunity in healthcare.
Take action in building organization capacity and advocate for community capacity building to:
Address contributors to chronic diseases –lifestyle/activity, behavioural health, and social needs
Optimize screening for chronic disease including metabolic syndrome– screening for high blood pressure, impaired fasting glucose, high triglyceride levels, abdominal obesity, high LDL levels, and low HDL cholesterol levels, as reported in The Global Epidemic of the Metabolic Syndrome.
Use screening data and other data (e.g., lifestyle/activity, behavioral health, social needs, demographics) to score everyone’s risk for chronic disease
Assure everyone identified as at-risk for chronic disease or with chronic disease has access to evidence-based lifestyle coaching, behavioral health services, and social need services, according to what Maria van Namen said in her article.
Accelerate broad adoption of evidence-based chronic disease care using best practices for physician engagement including data analytics that fosters co-opetition among physicians, as seen in Kaiser Permanent Program that Reduces Cardiovascular Disease Risks.
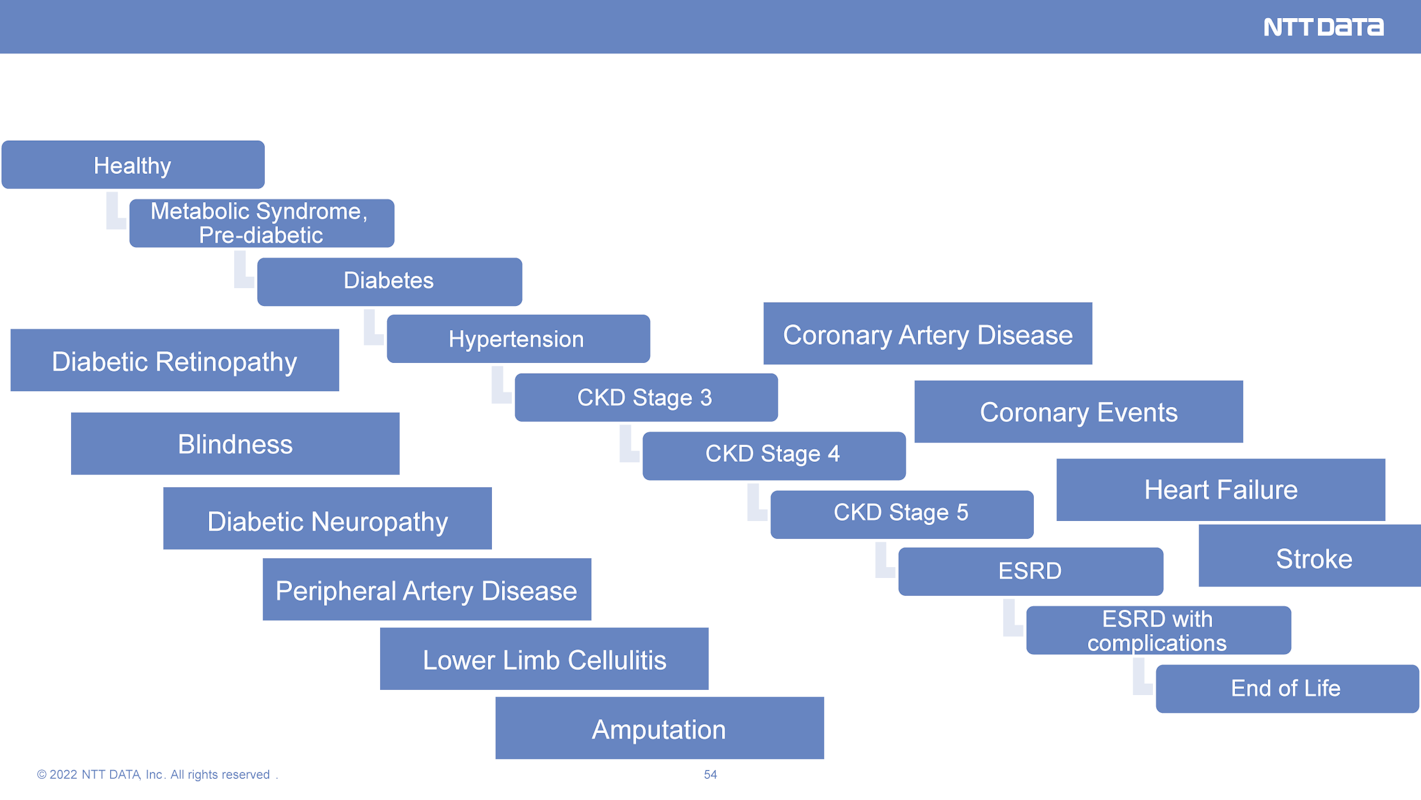
Measure the prevalence of chronic disease complication and comorbidity – work to innovate to minimize the cascade of complications and co-morbidity (See cascade below).
Provide care at home for homebound patients with a burdensome set of chronic care complications and co-morbidities, based on the success of the CMS CMMI Home-based Primary Care Pilots and Landmark Health.
And lastly, work with government and other public/private stakeholders to address healthcare worker shortages driven by aging populations and worker stress.
Header photo by Myriam Zilles on Unsplash
Subscribe to Our Newsletter
Get the latest insights about Global solutions for leading insurers on your email